Abstract
Introduction: Timely hospice enrollment is widely endorsed as an indicator of quality end-of-life (EOL) care. Although there have been significant increases in overall rates of hospice for patients with blood cancers, there have also been concomitant increases in "late" enrollment (generally defined as stays of ≤ 3 days before death). Such late enrollment may be less meaningful, as patients are being admitted to hospice primarily to manage their death, rather than to obtain additional palliative benefits. We aimed to characterize hospice use among patients with myeloma, focusing on prevalence and predictors of late enrollment.
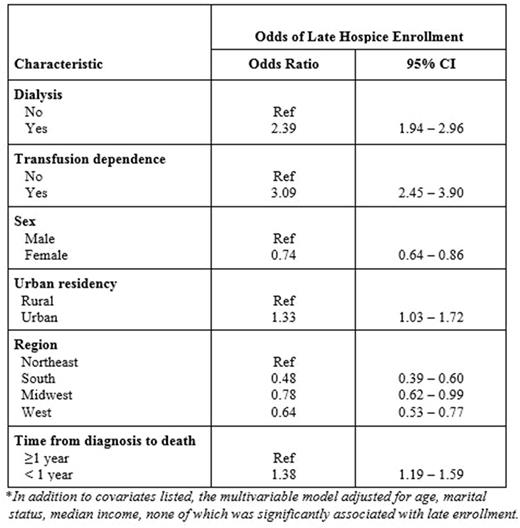
Methods: We conducted a retrospective analysis using the Surveillance Epidemiology and End Results (SEER)-Medicare database. Patients ≥ 65 years of age who had a primary diagnosis of myeloma between 2000 and 2013, lived for at least 30 days after their diagnosis, and died prior to December 31, 2013 were eligible for inclusion. We examined time trends in overall hospice use and late enrollment (defined as ≤ 3 days before death). Next, limiting our analysis to those who enrolled, we fit a multivariable logistic regression model to characterize factors independently associated with late enrollment, including sociodemographic and clinical characteristics (for those with p <0.05 in univariable analysis).
Results: A total of 12,803 patients with myeloma were eligible. Overall, 47.9% enrolled in hospice, of which the majority used outpatient/home hospice services (80.5%). The median length of stay in hospice was 12 days. Among those who enrolled, 17.8% spent ≤ 3 days in hospice before death. There was a significant trend in increasing hospice use from 28.6% in 2000 to 56.4% by 2013, p <0.001, but no significant increase in late enrollment (12% in 2000 to 16.7% in 2013, p=0.38). Transfusion-dependent patients (37.9% vs. 16.6%, p <0.001) and patients on dialysis (32.9% vs. 16.6%, p <0.001) were more likely to experience late enrollment, an association that remained significant in multivariable analysis. Other factors associated with late enrollment are shown in the Table below.
Conclusions: In this large cohort of myeloma decedents, there was a significant increase in hospice use over time, reaching a clear majority enrolling by 2013. Unlike many other hematologic cancers, gains in hospice use were not accompanied by increases in late enrollment. Distinct features of myeloma as compared to other blood cancers-such as incurability and high prevalence of pain at the EOL-may make the need for hospice services at the EOL more clear and encourage more timely enrollment.
Richardson: Takeda: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; Jazz Pharmaceuticals: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Oncopeptides AB: Membership on an entity's Board of Directors or advisory committees. Anderson: Bristol-Myers Squibb: Membership on an entity's Board of Directors or advisory committees; C4 Therapeutics: Other: scientific founder; Millenium Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; Oncopep: Other: scientific founder; Gilead Sciences: Membership on an entity's Board of Directors or advisory committees; MedImmune: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal